Three-dimensional anatomical models designed and printed at the University of Colorado Anschutz Medical Campus are helping surgeons in CU’s Department of Surgery perform breast reconstructions faster and more accurately. According to the university, the models have resulted in a 45-minute reduction in operating room time during surgeries.
Created by Nicholas Jacobson, a design researcher at CU innovation hub Inworks, the 3D-printed models specifically help surgeons performing a breast reconstruction procedure known as DIEP free flap, in which skin and fat from the lower belly, along with blood vessels, are transferred to the chest in order to rebuild the breast.
“DIEP free flap is a type of autologous breast reconstruction. During the procedure we take the excess tissue of the lower abdomen based on specific blood vessels called the deep inferior epigastric perforator,” says Christodoulos Kaoutzanis, MD, assistant professor of plastic and reconstructive surgery. “That vessel has smaller branches that deliver blood to the skin and fat of that region. For every patient, we isolate the most appropriate branches that will provide the best perfusion to the tissue we plan to transfer to the chest.”
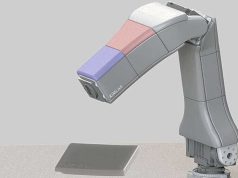
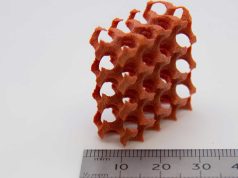
That decision is typically made using a CT scan, but the 3D model gives the surgeons a more accurate view of how the blood vessels are arranged and provides a resource they can use both prior to surgery and in the operating room. A unique model is created for each patient, based on their imaging.
“When you have the model, you not only get a better understanding of the trajectory of the vessels in three dimensions, but also you don’t have to go back and forth to your scan and waste time,” Kaoutzanis says. “You can just take a look at the model. We wanted to see if we could reduce the duration of surgery — and do that safely and effectively — using this method.”
Reducing time in the OR
The model-assisted procedure has proved a success since it debuted in the CU Department of Surgery in December 2021, reducing operating room time by 45 minutes and lowering surgical risk for patients.
“We had done a study where we randomized DIEP free flap patients to getting no scan at all, or getting a CT scan, and we demonstrated that the CT scan did reduce operative time,” says David Mathes, MD, chief and professor of plastic and reconstructive surgery. “We hypothesized that by using these 3D models, we could further reduce the operative time by enabling even better planning.”
Jacobson, who specializes in creating 3D replicas of human anatomy, had a hunch that 3D models would help with DIEP free flap surgery; working with CU surgeons, he developed 12 different models before finally arriving at the version that would best fit their needs. The models are created about a week in advance of the surgery and brought to the surgeons the morning of the procedure so they can familiarize themselves with the patient’s anatomy prior to surgery and map out the best path to take. Patients can even take the models home with them after the surgery if they want to.
“It’s almost like we take the CT scan and bring it to life when we bring it into three dimensions,” Jacobson says. “At first it was taking our team about 10 hours to produce a model. We’ve gotten that time down quite a bit, so now it takes about half that time. We can do this relatively quickly now.”
Training tool and further applications
In addition to serving as a valuable resource for surgeons during the procedure, the 3D models also have become an important training tool for surgical fellows, Jacobson says, allowing them to better visualize exactly how the surgery works.
“I hear a lot from the fellows who are learning to do this surgery who say the model is really helpful, just in their understanding of what’s going on,” Jacobson says. “It gives them a comprehensive view. A lot of students who are coming through now are so used to being able to see things in 3D; it’s part of their education. It really helps them.”
Now that 3D printed models have proven effective in breast reconstruction, surgeons are beginning to look at their potential in other surgeries as well, including eye surgery and gender-affirming surgery.
“We think this is just the tip of the iceberg of what we can do,” Jacobson says. “This is a wonderful study to prove that there is a benefit. The collaboration between a designer and a doctor is very powerful. It’s great to give them the power of design to create the tools they need. It seems like every time I meet with them, we talk about another avenue to go down.”
Find out more about the University of Colorado Anschutz at cuanschutz.edu.
Subscribe to our Newsletter
3DPResso is a weekly newsletter that links to the most exciting global stories from the 3D printing and additive manufacturing industry.